Infection control: How infections spread and who is at risk
The term infection control is something that healthcare workers in the UK should be aware of. Infection control is linked to all aspects of health, welfare, and personnel protection. GP surgeries, homecare, hospitals, and other healthcare services in the UK continue to ensure the management and implementation of infection control strategies throughout their premises, thus making it a key component in the provision of the services.
There are mainly 3 types of infections that individuals are more likely to experience at some point in their lives. These include bacterial, viral, and fungal infections. Infection control management is part of an overall management system and is thus common across various industrial sectors in the UK.
What is infection control?
Infection control is the science of preventing infections in healthcare settings. A pathogen or infection is a biological agent that causes disease or illness in its host. Pathogens cannot be seen with the naked eye and therefore present increased difficulty in controlling and managing potential outbreaks of infection.
Management is responsible for ensuring that its workforce is adequately trained. This should be specific to the healthcare setting in terms of the potential presence of pathogens and the prevention of their spread. This includes all personnel, such as those who provide direct services like doctors, nurses, GPs, and dentists, as well as those who provide support services like contractors, cleaners, kitchen staff, and so on.
However, educating personnel is difficult due to varying levels of understanding, but the most difficult challenge is often providing adequate risk mitigation strategies for visitors who may introduce pathogens into the workplace environment.
Why can infections be dangerous?
Infections can be extremely dangerous because they cause toxins to be produced in the body. They reproduce quickly, which can cause parts of the body to malfunction when the infection attacks the body. This causes damage to the organs and other parts of the body where the infection is.
How are infections transmitted?
There are 4 ways in which infections are spread, and they are as follows:
1. Direct transmission
This type of transmission occurs when two people make physical contact. Often, family, friends, and colleagues will be susceptible to direct transmission, as they are in close contact with you. Another method of transmission is through the placenta from a mother to her unborn child. Transmission can occur through cuts or scratches and through body fluids such as blood, saliva, and vomit.
2. Indirect transmission
When the transmission does not involve physical contact, such as airborne transmission. This occurs when droplets are in the air, but they don't immediately disappear and remain there for some time after. Contaminated objects such as door handles, computer keyboards, light switches, and so on can also be sources of indirect transmission.
3. Food
When consumed, food that has not been properly cooked can cause bacteria to grow and multiply inside our bodies. When people consume this food, it can cause them to develop an infection. This is also true of dirty water; if the water contains bacteria that the body has never encountered before, it can cause the body to become ill.
4. Environmental reservoirs
Soil, water, and plants can also have microorganisms that make people sick. These microorganisms can spread to people through drinking water or by touching them directly.
Who is most at risk of infection in the UK?
Everyone in the community is at risk of developing an infection; however, there is a certain more vulnerable group. These include people who are already unwell due to other diseases; their immune systems will already be weaker than normal, and they could easily pick up another infection.
People who are elderly or very young, those undergoing treatment requiring the use of medical equipment, those who are malnourished, and pregnant women are also at a higher risk of infection.
In the UK, the NHS has given advice on how to cut down on the risk of spreading infections in healthcare settings. They are known as the general principles of infection prevention and control, which are designed to reduce risk and protect both carers and patients. The principles cover everything from hand hygiene to chemical waste disposal.
What are the general principles of infection prevention and control in the UK?
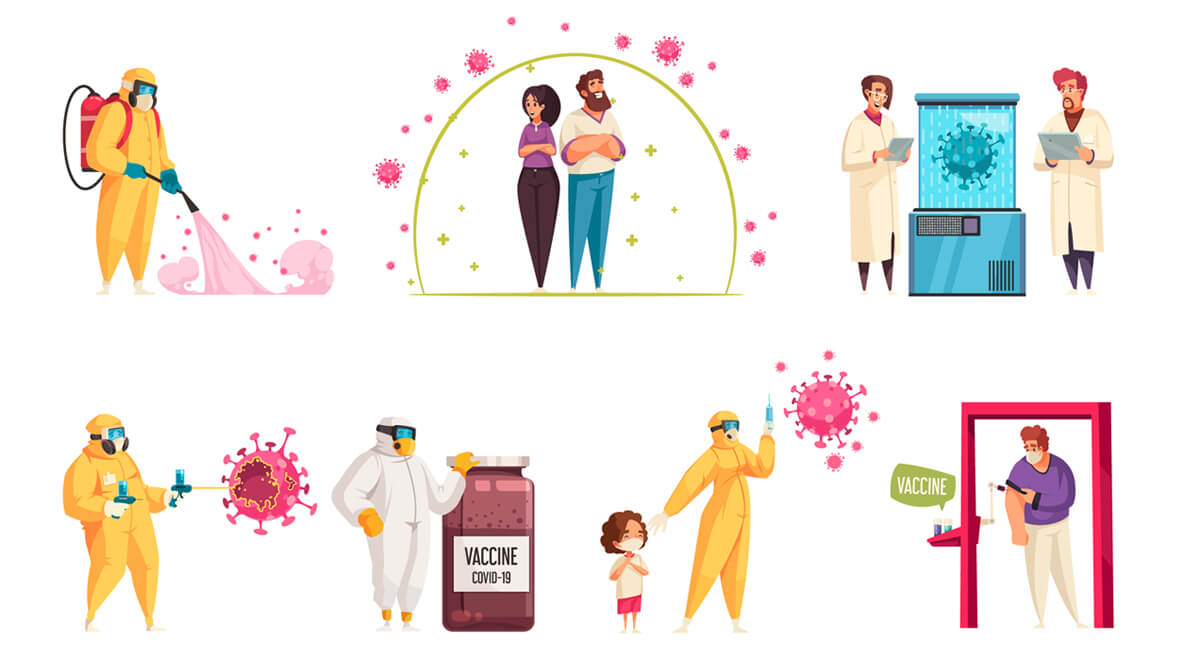
The general rules for preventing and controlling infections must be used in all patient care in the UK. They are a set of common practises that, if followed, will prevent the spread of infection between patients and care providers, as well as between patients themselves. The general infection control principles in the UK include the following:
1. Hand hygiene
2. Using personal protective equipment (PPE)
3. Handling and disposal of sharp objects safely
4. Safe handling and disposal of chemical waste
5. Managing blood and body fluids
6. Decontaminating equipment
7. Achieving and maintaining a clean clinical environment
8. Appropriate use of indwelling devices
9. Managing accidental exposure to blood-borne viruses
10. Effective communication
11. Training
Infection risk assessment
To keep people safe, it is important to figure out how likely someone is to catch or spread an infection and give them information about it. Before a person in the UK uses a healthcare service, their risk of getting an infection should be looked at. This assessment will help make the care plan by letting us know if we need to take any extra steps to prevent and control infections, like isolating the patient or giving them more PPE.
The assessment must include all factors that put the person at a higher risk of catching or spreading infection, which includes recording their symptoms (fever, unexplained rash, etc.), contact (recent travel outside the UK where there is infection or contact with people with infection, etc.), and personal risk factors (wounds, environmental risk factors, etc.).
1. Reducing risk
The hierarchy of controls is a system used to reduce chance at work. For social care settings, the hierarchy control principles can be broadly interpreted as follows:
2. Reducing the hazards
In the UK, public health measures such as vaccination, testing, and isolation help reduce the risk of infection. Taking vaccination shots for flu and COVID-19 can help reduce the risk. However, it won't work when ill; advising people to isolate while infectious and recognising and reporting infections help reduce the transmission.
3. Changing what we do
When faced with a particular risk, such as an outbreak, we must change the way we do things, such as reducing communal activities, adding disinfectant to cleaning, etc., to help reduce the spread of infection.
4. Changing where we work
After COVID-19, working from home (WFH) has become the new normal. When WFH is not possible, it is always advisable to make your workplace safe.
5. Changing how we work
Changing the way we organise work can reduce risk, such as by reducing the number of people in a space at any given point in time. Also, administrative controls such as risk assessments, training, audits, etc. also help to reduce the chance of infection at work.
Nurses Group Homecare in Yeovil, UK, follows all the infection control and prevention procedures so that both our clients and carers are safe. We provide homecare staff with infection control training so that they follow all the safety procedures.